The Workplace Athlete
An alternative approach to musculoskeletal injury prevention and worker health and well-being
Abstract
For decades, occupational safety and health professionals have sought to mitigate musculoskeletal disorders (MSDs) through traditional ergonomic risk factor analysis and workstation design. Despite these efforts, MSDs; continue to plague nearly all work environments. While there have been innovative solutions developed over the last century that have reduced MSDs, these have primarily resulted from ergonomic workstation redesign, awareness training, and medical case management. This area of injury prevention has shown to be complicated and continues to present implementation difficulties due to natural anthropometric variations of workers’ physiological capabilities. This study examines this problem from a different point of view. In addition to designing neutral workstations, addressing and improving individual worker musculoskeletal, mobility, stability, and flexibility, particularly in critical anatomical joints, has significant potential for enabling worker self-conditioning, much as an athlete would undergo physical conditioning to perform physical tasks without injury, even when presented with pre-existing physiological limitations. The objective of this article is to report on data collected and analyzed, then evaluate what, if any, trends can be understood from the FMS assessment measurements when applied in a pre and post-application in combination with a set of mobility-based exercises. This analysis seeks to answer the following research questions: Does the alternative movement improvement program model improve worker physiological condition measured by the Functional Movement Screen? Does the movement improvement model impact musculoskeletal injury prevention efforts? The authors hope to demonstrate movement-improvement programs as a viable complement to traditional Ergonomics and Musculoskeletal Disorder prevention programs.
Introduction
An alternative approach to musculoskeletal injury prevention and worker health and well-being
For decades, occupational safety and health professionals have sought to mitigate musculoskeletal disorders (MSD) through traditional ergonomic risk factor analysis and workstation design. Despite these efforts, MSDs continue to plague nearly all work environments. Since the first publication in 1857 of “An Outline of Ergonomics, or the Science of Work” by Wojciech Jastrzebowski (Jastrzebowski, 1857), scholars, researchers, and practitioners alike have sought to utilize anthropometric, physiological data, medical science, and engineering principles to improve the worker experience, increase productivity, and lessen the potential for injury. While one might assume the problem is centered around work tasks with substantial physical activity or repetitive type work, employees in sedentary workplaces suffer not only injuries, but physical discomfort and health degradation due to the lasting effects of poor body mechanics. According to the Bureau of Labor Statistics, 31% of all workplace injuries in the private sector in 2018 were related to overexertion and bodily reaction resulting in MSDs (BLS, 2018).
Additionally, the United States Bone and Joint Initiative reported in 2016 that an estimated 127 million Americans are affected by musculoskeletal conditions, and these disorders cost an estimated $213 billion in annual treatment, care, and lost wages. Furthermore, there has been much recent public discourse centered on medical research reporting the adverse health effects of a sedentary lifestyle, including metabolic dysfunction, vascular degradation, and bone density reduction. These types of physiological effects can result in diseases such as obesity, diabetes, cancer, heart disease, stroke, and psychosocial disorders (Tremblay, et al., 2010).
While there have been innovative solutions developed over the last century that have reduced MSDs, these have primarily resulted from ergonomic workstation redesign, awareness training, and medical case management. This area of injury prevention has shown to be complicated and continues to present implementation difficulties due to natural anthropometric variations of workers’ physiological capabilities. Additionally, some work tasks simply cannot be redesigned to improve ergonomic neutrality due to the transitory or temporary nature of the work. With the recent changes in virtually all work environments due to the COVID-19 pandemic, there will likely be increased instances of working from home and transient workstations rather than permanent desk or office configurations, further exacerbating this problem.
Beyond the office-based setting, work tasks, specifically in construction, maintenance, medical, and emergency response domains, present unique and challenging ergonomic risk factors such as awkward postures, over-exertion, and joint hyperextension or flexion. These tasks are challenging to redesign and modify due to their temporary and sometimes urgent nature with an ever-evolving work activity zone that does not replicate itself on a routine basis—such as the case in more static environments found in manufacturing or assembly line work. For example, welders must often position themselves in cramped or awkward spaces to reach the material’s face that must be welded. Utility workers often reach and stretch their extremities to access a point of attachment for pipelines, electrical conduit, or wiring. Many times, workers are restricted in excavations or confined spaces or elevated in aerial lift equipment. Firefighters and emergency medical responders operate in a crisis environment where time is essential to the successful recovery of a victim. They must move quickly, sometimes awkwardly, to either reach a victim or remove them to safety for further assessment and treatment. Medical professionals in trauma centers, intensive care units, and other exigent medical scenarios must move swiftly, sometimes wrestling an unconscious patient to place them in an optimal position for treatment.
Adding to this dilemma are regulatory restrictions placed on workplaces in the United States that prohibit discrimination and utilization of personal medical information to assign workers to job positions based on physical ability. While the Americans with Disabilities Act (ADA) does allow for reasonable accommodation, the reality of accommodating workers with minor movement disorders is problematic, if not impossible, due to the individuality of each person’s specific physical condition (Americans with Disabilities Act, 2008). It should be noted that the methods described herein are not intended to be utilized as a pre-employment screen or physical capacity evaluation for placement into an employment position or post-injury medical case management, but rather as a movement assessment to evaluate mobility restrictions and identify areas for individual improvement. Any implementation related to employment or job placement should be done so in consultation with human resources and legal professionals specializing in fair labor practices.
This study examines this problem from a different point of view. In addition to designing neutral workstations that accommodate 96% of the anthropometric population, addressing and improving individual worker musculoskeletal, mobility, stability, and flexibility, particularly in critical anatomical joints, it has significant potential for enabling worker self-conditioning, much as an athlete would undergo physical conditioning to perform physical tasks without injury, even when presented with pre-existing physiological limitations.
The data for this study was collected by a human movement and physiology clinic specializing in novel musculoskeletal injury prevention programs. This particular clinic focuses on best practices in sports medicine and human movement performance and has collected thousands of points of movement data from multiple industrial domains relative to worker joint stability and mobility through a biomechanical assessment called the “Functional Movement ScreenTM” (FMS™). The FMS is an assessment method commonly used in physiological domains such as physical therapy, rehabilitation, sports medicine, and chiropractic practices. The FMS assessment consists of evaluating a series of movements and joint articulation, similar to those used in physical therapy and elite and professional athletic training (Cook, et al., 2006). First developed by Boyle and Coyle as the “joint by joint” concept for the application of physical therapy practices (Boyle & Verstegen, 2012), the FMS functions as an assessment used to measure motor and stabilization skills, grade baseline movement patterns, and determine the existence of movement restriction, mobility asymmetry, or pain with movement. (Bonazza, et al., 2017). The FMS baseline assessment is then combined with mobility-based exercises to improve individual worker joint movements and resilience to injury and then followed up with subsequent assessments to track mobility improvement.
The objective of this article is to report on the data collected and analyzed, then evaluate what, if any trends can be understood from the FMS assessment measurements when applied in a pre- and post-application in combination with a set of mobility-based exercises. This analysis seeks to answer the following research questions: Does the alternative movement improvement program model improve worker physiological condition measured by the FMS? Does the movement improvement model impact musculoskeletal injury prevention efforts?
The Worker is an Athlete
A significant percentage of sports and orthopedic injuries are related to overuse syndromes caused by the repetitive nature of a specific joint movement. These injuries are typically similar to those that occur in industrial workplaces because of their repetitive nature (Sevier, 2000). Since the term “workplace athlete” was first identified in 1985, the argument holds that workers should be assessed and treated for injuries like athletes (Rozmaryn, 1996). This concept is relevant in two critical areas; workers should be physically conditioned for the job/tasks they are expected to perform to potentially prevent injury and improve workplace performance (Amtmann, 2016).
Additionally, workplace athlete programs can enhance or sustain worker health and wellness and quality of life. It has been observed that an athlete’s repetitive mechanical movements are precursors to sports-specific injuries due to increased stress on tendons, ligaments, and joints. Similarly, many physical movements performed repetitively on the job site by the worker/laborer often result in the same type of injuries that an athlete will suffer (Viola, 2020).
Research Methods
Working with participating client organizations, pre- and post-assessment data was collected on a variety of types of workers in the following industries: electrical and gas utility, wind turbine operations, food manufacturing, shipyards, mining, construction, oil refining, warehousing, HVAC and plumbing, fire/security alarm installation and maintenance, and customer service call centers. Workers participating in these assessments ranged in age from early twenties to sixty-plus and encompassed a broad spectrum of physical ability from a sedentary lifestyle to physically active. This research project analyzed and aggregated the de-identified data collected from 1,495 participants from 19 different companies across 12 various industries. Informed consent and a waiver for anonymous data release were obtained from each subject before data collection and participation in the program. Authorization was received from participants to review blind assessment scores and aggregate data for research purposes.
Functional Movement Screen
The FMS analyzes unique movement patterns without consideration of weight or repetition. The central goal of the FMS assessment is to detect deficiencies in biomechanics, and clinicians consider the tool to be more reliable than conventional stretching movements. The FMS includes seven specific movement evaluations, which require an appropriate movement of the body’s kinetic linking system. The kinetic link model, used to analyze motion, depicts the body as a linked system of interdependent segments. Each of the FMS movements detects movement on distinct parts of the body (Cook, Burton, & Hoogenboom, 2006a).
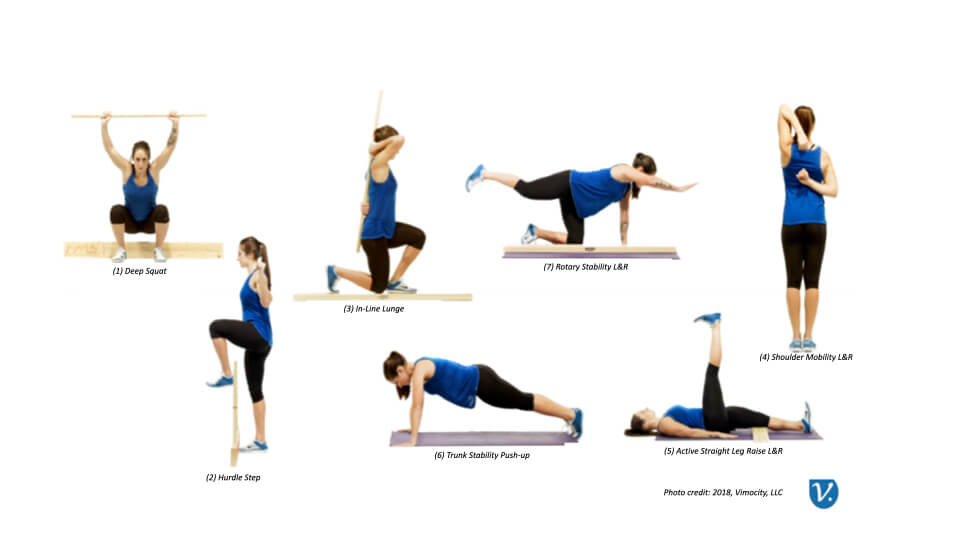
The movements in the assessment are as follows: (1) deep squat, (2) hurdle step, (3) in-line lunge, (4) shoulder mobility, (5) active straight leg raise, (6) trunk stability push up, and (7) rotary stability (Figure 1). The deep squat and hurdle step movement assesses bilateral, symmetrical, functional mobility of the hips, knees, and ankles. In contrast, the in-line lunge assesses hip and ankle mobility and stability, quadriceps flexibility, and knee stability. The shoulder mobility screen considers a bilateral range of motion, combining internal rotation with adduction and external rotation with abduction. The active straight leg raise tests the ability to isolate the lower extremity from the trunk while maintaining the torso’s stability. The trunk stability push-up focuses on stabilizing the spine during upper body movement (Cook, et al., 2006b). FMS allows evaluators to determine baseline primal movement ability to develop improvement plans for individual movement patterns (Bushman, et al., 2016). The screen consists of seven movements that identify vulnerability in joint movements. These primal movement patterns provide an observable presentation of basic locomotor movements. The tests place the participant in extreme bodily positions where weaknesses and imbalances become noticeable if appropriate stability and mobility are not utilized (Cook, et al., 2006a).
The seven movements encompass the major joint and muscle groups susceptible to musculoskeletal disorders. The seven individual movement tests are then individually scored on a scale from 0 to 3, with the highest composite score achievable at 21 and the lowest possible score at 0. Clinicians and researchers have established that an FMS score below 14 is considered deficient, and the individual presents a poor function in the targeted area of each movement (Cook, et al., 2006b). A risk assessment model was applied to the total score with 0-11, indicating the highest risk of mobility difficulty, a total score between 11 and 13 indicating a moderate risk of mobility difficulty, and a score higher than 14 indicating the lowest risk of mobility difficulty. It is noted that an FMS score of 2 on any singular movement demonstrates that the movement was executed without the subject reporting pain, although some compensations were detected. Furthermore, a score of 1 indicates that the subject could not perform the movement task within the designated parameters. Subsequently, a score of 14 would mean that a person could complete all seven motions with only minor compensations, no pain, and no asymmetrical movement (Rindal, 2018).
The use of the FMS as a predictor of musculoskeletal injury is controversial. Research studies in professional and elite athletic therapies have yielded contradicting results in terms of the assessment’s ability to measure the potential for injury risk accurately. NFL players with FMS scores less than or equal to 14 had an increased chance of injury than players with scores higher than 14 (Kiesel, et al., 2014). Furthermore, studies in athletes performing overhead motions such as tennis or volleyball, which could be assimilated to overhead industrial work performed by electricians, plumbers, and pipe installers, could benefit from a pre-activity assessment tool such as the FMS in combination with training and conditioning programs utilized as mitigative tools in the prevention of shoulder injuries (Cools, et al., 2015). However, later research into the assessment’s efficacy did not provide a reliable predictor of sports injury (Philp, 2020).
It is important to note that the FMS should not be utilized as a standalone tool for injury risk prediction; it should be used in combination with a case history of pain and previous injury. Medical case histories, if collected, should be conducted by a licensed healthcare professional. While the FMS has been used for professional and elite athletes, along with military and emergency response personnel, to determine the extent of how susceptible an athlete is to receive an injury, the predominant conclusion was that the FMS alone was most effective at determining a dysfunctional fundamental movement pattern, which could be a precursor to joint degradation or injury, but was inconsistent in predicting the injury itself with any reliability (Philp, 2020). Furthermore, individual components of the FMS may be a better predictor of injury in targeted joint combinations than the overall composite score (Armstrong & Greig, 2018). Previous studies have shown that FMS has high interrater reliability (Cohen’s Κappa > 0.85) when assessment technicians are trained and follow the standard procedure for conducting the test (Minick, et al., 2010). In the data collection for this study, FMS assessments were conducted by qualified physical therapists and sports management professionals trained in the FMS assessment procedures.
Two more elements that were considered along with the FMS assessment were pain levels and breathing patterns. Research in military populations suggests that the experience of pain during the FMS had an equal predictive ability with injury risk when the total score was less than 14 points. Soldiers who experienced pain on any of the seven movements were significantly more likely to experience an injury than those who scored the highest point in any individual category (Alemany, et al., 2017). Additionally, breathing mechanics play a crucial role in total body movement. Breathing Pattern Disorders (BPD) have been shown to contribute to pain and motor control deficits, resulting in dysfunctional movement patterns and subsequent injury. Effective breathing patterns are known to contribute to overall movement health. Individuals who exhibit BPD signs are significantly more likely to score poorly on the FMS (Bradley & Esformes, 2014). Further analysis and developments in physiotherapy protocols have informed a multi-faceted approach with an injury prediction algorithm encompassing not only the FMS score but an assessment of any previous injuries, the presence of pain during the evaluation, detection of asymmetry during the evaluation, and analysis based on gender and activity levels (Plisky, 2015).
Results
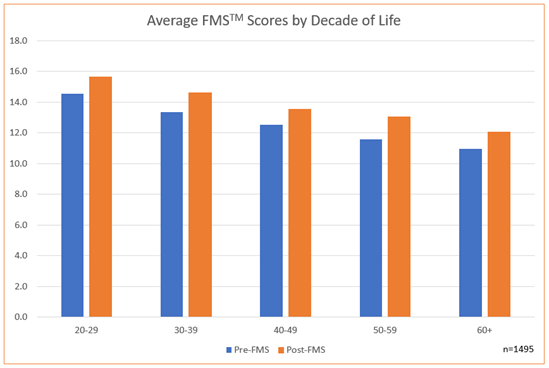
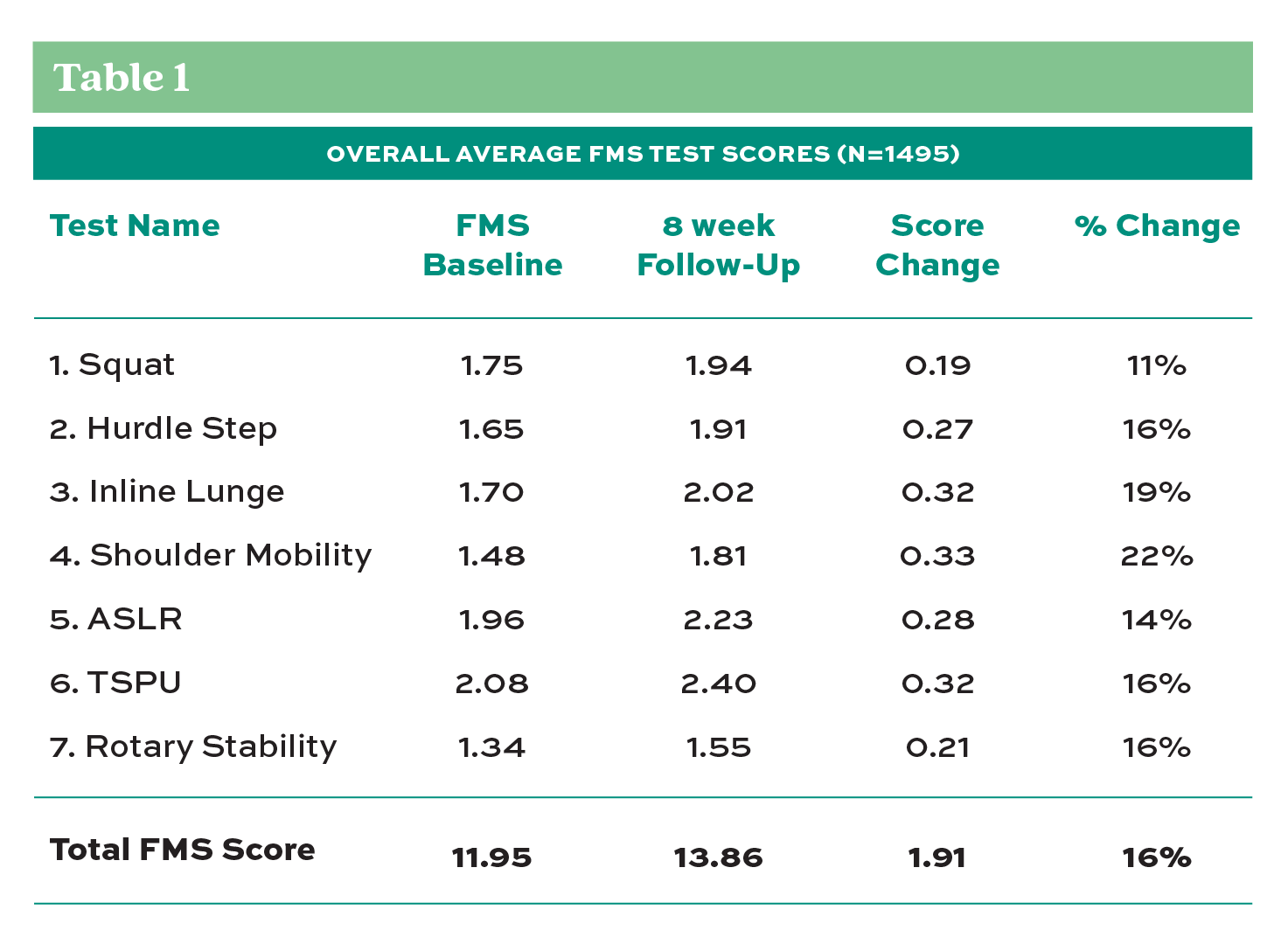
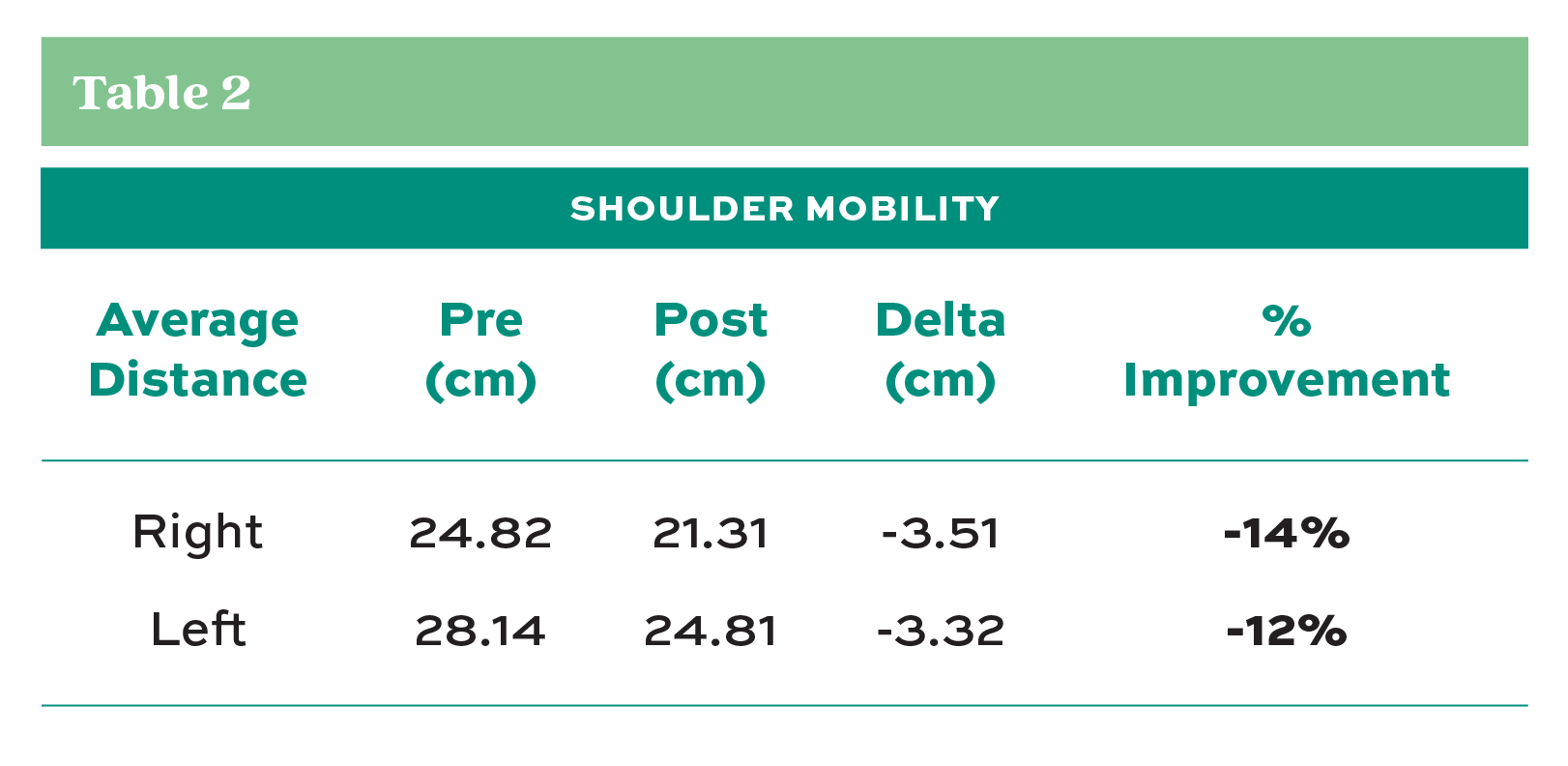
Analysis of pre-and post-assessment scores revealed encouraging results. In the individual FMS test criteria, improvements were noted in the participants’ average scores in each movement category (Table 1) after eight weeks of daily self-care routines. Furthermore, when evaluated by participant age, every decade of life category showed improvement in the average score from pre- to post-assessment (Chart 1). The most significant improvement in the individual test score averages occurred in the shoulder mobility test with 22% improvement, while the overall average FMS score improved 16%. Table 2 shows that the average shoulder mobility improvement scores in both the left and right shoulders were 12-14%. The shoulder mobility test measures the distance (cm) between the hands from the distal wrist to the third digit’s tip in the opposite hand when the subject reaches behind their back, attempting to touch their opposite fingers together (see Figure 1, item 4). Shoulder mobility is important because studies have shown that a shoulder internal rotation deficit is a predictor of a shoulder injury (Cools, et al., 2015).
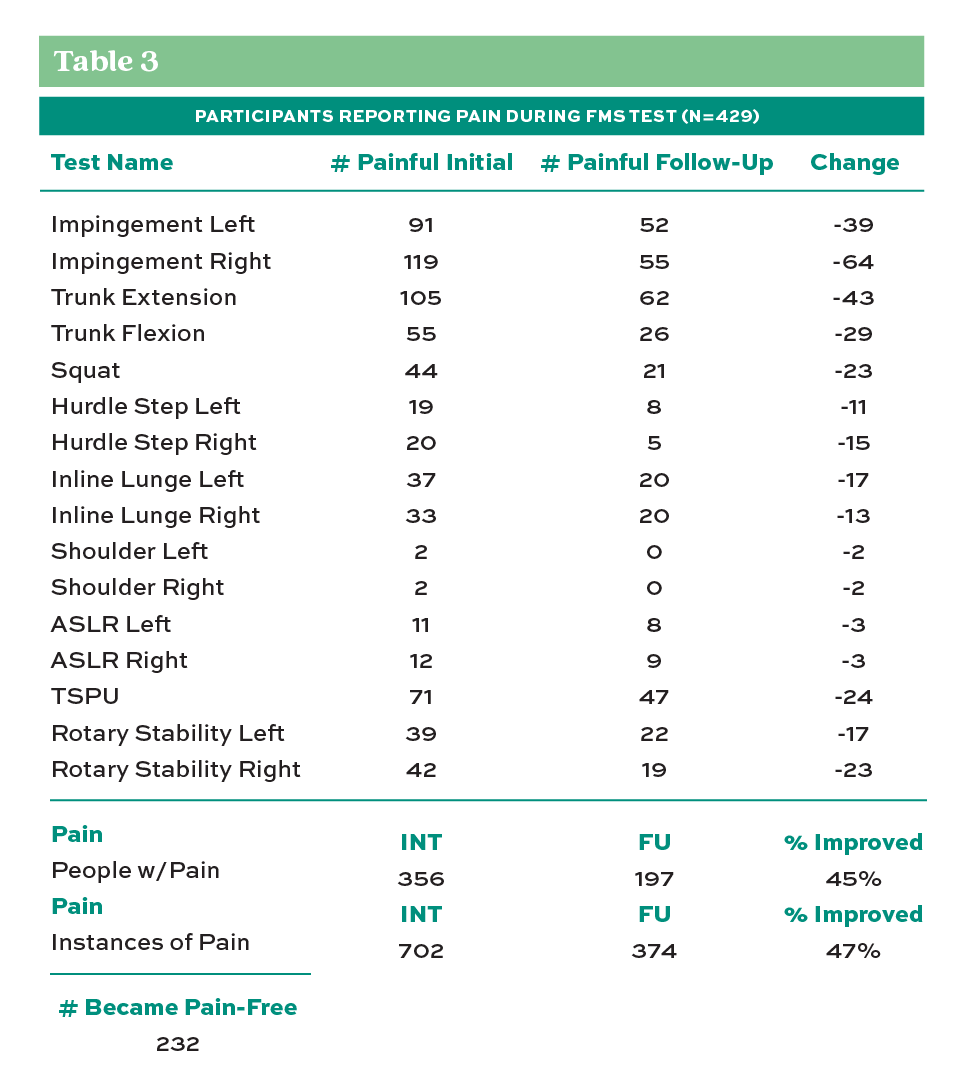
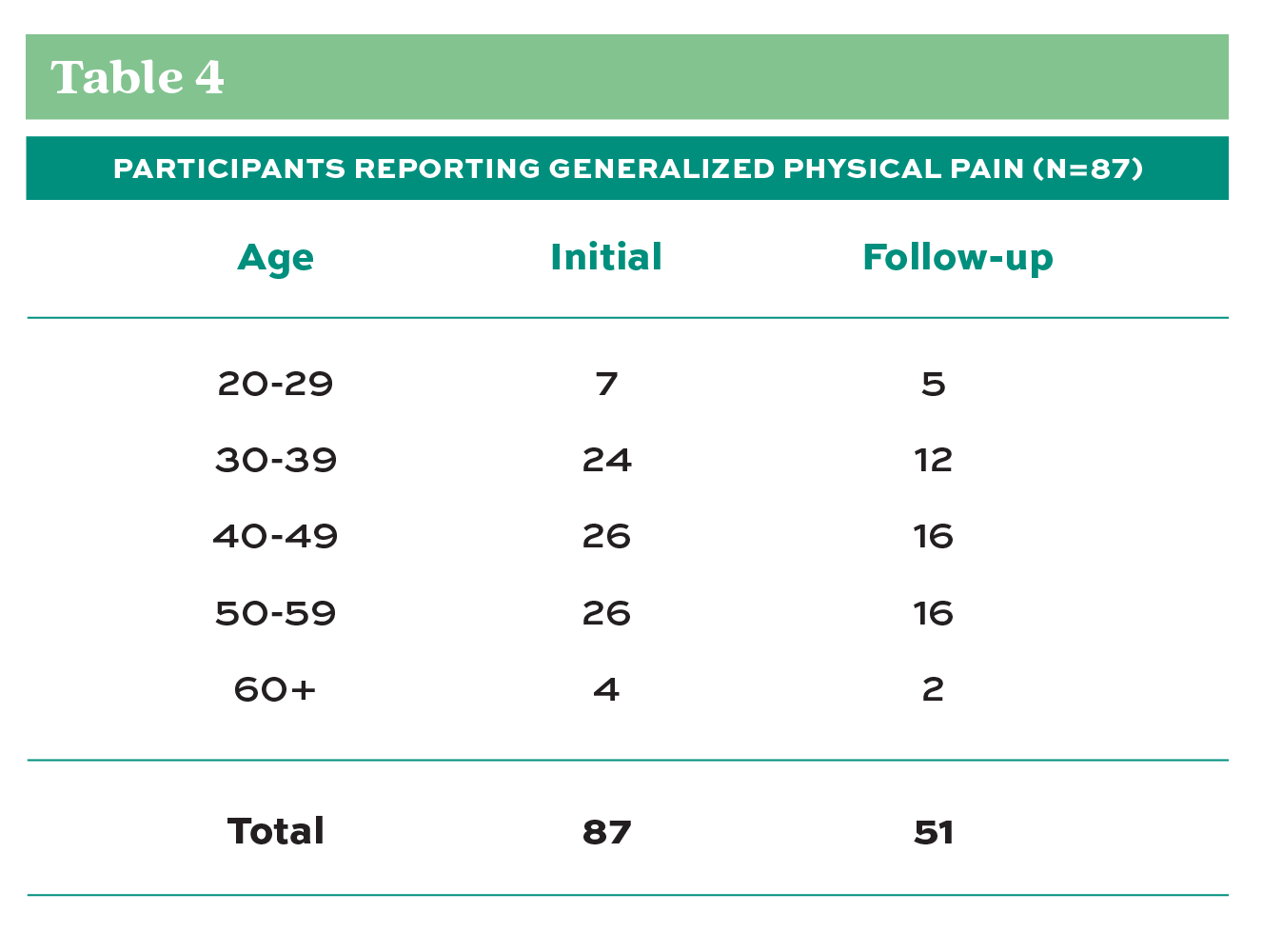
Concerning pain indicators during pre- and post-testing, both Table 3 and Table 4 show that those participants who reported pain during the pretest, on average, showed less reporting of pain during the post-test after the eight-week self-care program. The number of people reporting pain and the number of pain instances during the test showed a 45-47% improvement from the pre-test to the post-test. Given Alemany’s results that previous injury and pain experience during FMS are valid predictors of future injury (Alemany, et al., 2017), this finding provides significant evidence supporting the possibility of using this program as a valuable tool for the prevention of injury and improvement of worker comfort and well-being.
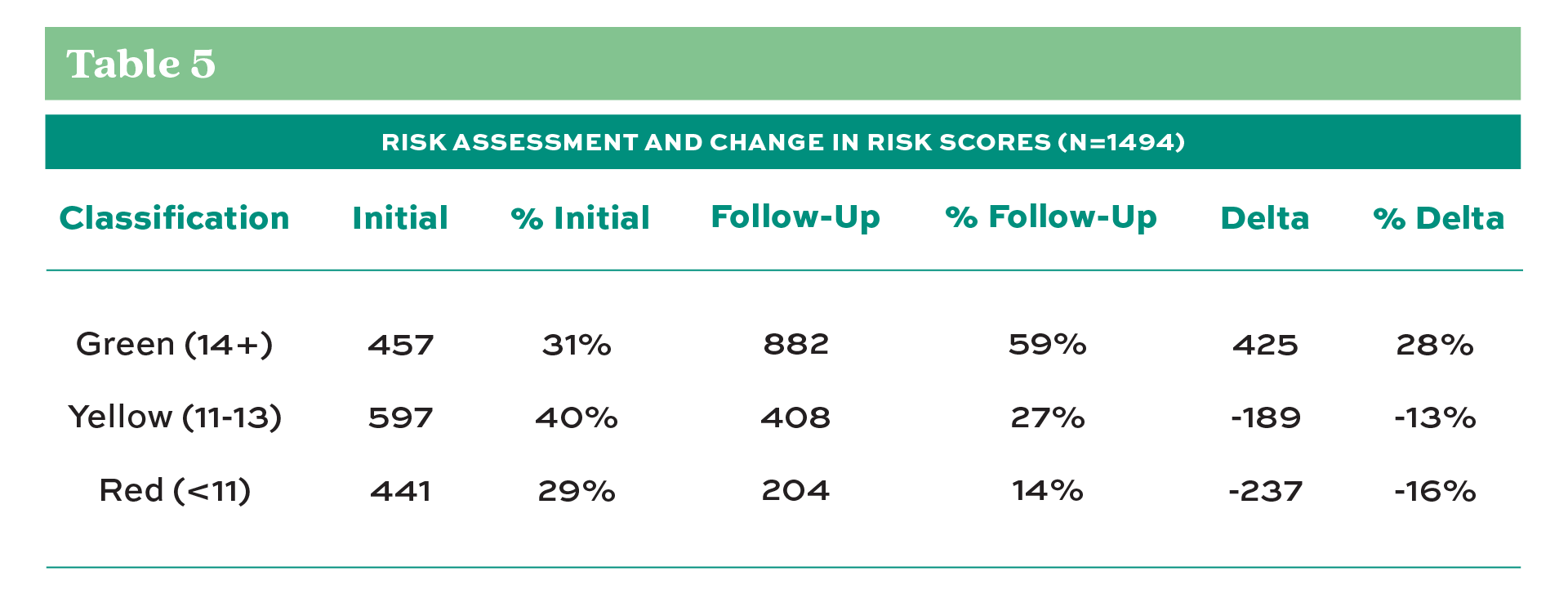
Finally, Table 5 reflects the difference in assigned risk between the initial testing to the follow-up. A 28% increase in individuals scoring above 14 was considered low to moderate risk and a 13% decrease in those scoring between 11-13, or moderate risk. Finally, those individuals identified as high risk with less than a score of 11 decreased 16% by increasing their overall mobility and moving into a lower risk category.
Discussion
Analysis of this collected data provides encouraging results concerning the ability to use FMS with an extended movement-improvement conditioning program combined with breathing improvement and pain awareness education. A case study conducted over three years with a single employer in the electric and gas utility company revealed favorable outcomes. This organization reported a 95% savings reduction of direct costs of sprains and strain injuries during the evaluation period. Additionally, this company reported an 81% increase in employee participants classifying as low risk (FMS score >14) for injury after participating in the program. Furthermore, the employer reported that 87% of employees who participated in the program had fewer days missed from work as compared to those workers who did not participate in the program, and 98% of the employee participants would recommend the program to a peer and was generally favorable in their assessment that this program is one part of a more extensive, robust safety and health management system (Rindal, 2018).
Much of the previous clinical research has focused on athletes and military members and anthropometric populations typified by healthy, physically fit, predominantly male, and between the ages of 17-30 years. This point is problematic when considering that the American workforce represents a much broader demographic. However, the data collected here were performed on a broad spectrum of industrial and office-based workers and clearly showed that improvement in mobility and pain awareness could be achieved by participating in self-care movement improvement routines in all age groups. Another anecdotal outcome reported by the FMS test administrators was that participants became more aware of their movement, flexibility limitations, and capabilities through their pre-test scores, even in seemingly “healthy and fit” participants (Cornell, 2020). Those participants became motivated to improve and participate even further.
Implementation of the Workplace Athlete Movement-Improvement Program

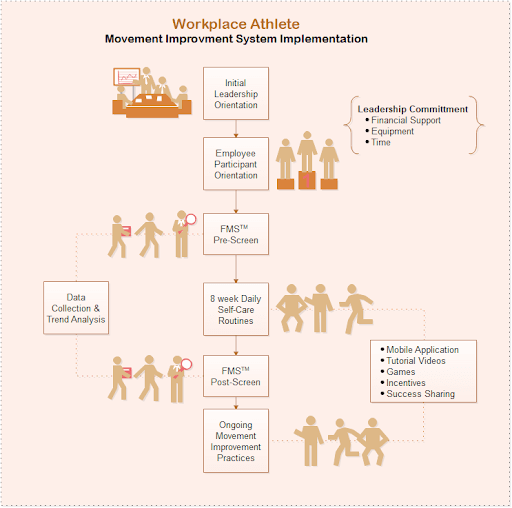
The Workplace Athlete Movement Improvement program is a long-term, sustainable program designed to encourage employees to improve their overall mobility and stability condition. Using adapted tools from physical therapy, chiropractic care, and sports medicine, the movement improvement program described herein combines assessment with regular movement, joint stability, and flexibility exercises. The program begins with an orientation session for employees and organizational leaders to help them understand the fundamentals of movement, flexibility, breathing, and the connection with the potential for MSD injuries. Participating employees are administered a baseline FMS assessment to determine their baseline score (0 to 21) and given instruction and essential tools to perform “Daily Body Care” movement exercises, including a 5 to 10-minute routine focusing on breathing, self-soft-tissue mobilization with a massage roller, and small movement mobility exercises (Figure 2). After the initial eight weeks, a second FMS assessment is administered to the participating employees to assess mobility improvements. During the first eight weeks, employees are encouraged to participate with recommended “Daily Body Care” mobility routine and are given additional specific recommendations based on individual mobility restrictions discovered in the FMS. Additional resources such as web-enabled applications, motivational and educational videos, corporate incentives, competitions, and success story sharing (Figure 3) sustain employee motivation over the length of the program. After the initial eight-week period, employees are encouraged to continue engaging in self-care exercises, share their successes and challenges, and encourage even more employees in the organization to participate. The long-term success of any specialized workplace injury prevention program requires total commitment and support from leadership in terms of time and resources to allow employees to participate in the pre- and post-assessment screening, the daily self-care exercises, and experience sharing across the organization.
Application of Movement Improvement programs in a post-COVID-19 World
Since the declaration of the COVID-19 pandemic and subsequent crisis response implemented in healthcare institutions across the globe, a concern has arisen about the physical well-being of the myriad of doctors, nurses, and other health care professionals tasked to work long hours in sometimes grueling conditions to care for the thousands of patients suffering from the coronavirus disease. A recent multinational study of healthcare workers found that approximately 50% of healthcare workers screened tested positive for moderate to very severe psychological distress after extended hours/days treating patients. There was a strong association between physical symptoms and psychological distress (Chew, et al., 2020). There may be opportunities in the health care field to utilize a program similar to the movement and breathing improvement programs described herein as preventive mechanisms to help medical professionals exercise self-care actions to cope with the severe working conditions they face during this pandemic crisis.
Conclusion
Ergonomic risk factors and musculoskeletal disorders such as sprains and strains continue to plague workplaces, regardless of industry type. The adverse effects of poor body movement and sedentary lifestyles only exacerbate the problem. This data analysis examined whether the alternative movement improvement program model could improve worker physiological ability as measured by the FMS. Would a movement improvement model impact musculoskeletal injury prevention efforts? While the results demonstrate that participation in a program does yield improvement in overall mobility and reduction in reported pain, anecdotal and case study evidence suggests a connection between movement improvement and prevention of injury. In the meantime, safety and health practitioners could utilize this or a similar program as another tool in their toolbox for risk assessment and mitigation. Movement-improvement concepts as a means toward worker health and well-being have broad applications in many workplace domains. Any workplace where people are required to sit, stand, and move could benefit from applying a program similar to what has been described herein.
References
Alemany, J. A., Bushman, T. T., Grier, T., Anderson, M. K., Canham-Chervak, M., North, W. J., & Jones, B. H. (2017). Functional Movement Screen: Pain versus composite score and injury risk. Journal of Science and Medicine in Sport, 20, S40–S44. https://doi.org/10.1016/j.jsams.2017.08.001
Amtmann, J. (2016). The Industrial Athlete and Flexibility. Primary Healthcare: Open Access, 06(01), 1–3. https://doi.org/10.4172/2167-1079.1000220
Armstrong, R., & Greig, M. (2018). INJURY IDENTIFICATION: THE EFFICACY OF THE FUNCTIONAL MOVEMENT SCREEN IN FEMALE AND MALE RUGBY UNION PLAYERS. International Journal of Sports Physical Therapy, 13(4), 605–617.
BLS, B. of L. S. (2018). Survey of Occupational Injuries and Illnesses Data.
Bonazza, N. A., Smuin, D., Onks, C. A., Silvis, M. L., & Dhawan, A. (2017). Reliability, Validity, and Injury Predictive Value of the Functional Movement Screen. American Journal of Sports Medicine, 45(3), 725–732. https://doi.org/10.1177/0363546516641937
Boyle, M., & Verstegen, M. (2012). Advances in functional training: training techniques for coaches, personal trainers and athletes. BookBaby.
Bradley, H., & Esformes, J. (2014). BREATHING PATTERN DISORDERS AND FUNCTIONAL MOVEMENT. International Journal of Sports Physical Therapy, 9(1), 28–39.
Bushman, T. T., Grier, T. L., Canham-Chervak, M., Anderson, M. K., North, W. J., & Jones, B. H. (2016). The Functional Movement Screen and Injury Risk: Association and Predictive Value in Active Men. American Journal of Sports Medicine, 44(2), 297–304. https://doi.org/10.1177/0363546515614815
Chew, N. W. S., Lee, G. K. H., Tan, B. Y. Q., Jing, M., Goh, Y., Ngiam, N. J. H., Yeo, L. L. L., Ahmad, A., Ahmed Khan, F., Napolean Shanmugam, G., Sharma, A. K., Komalkumar, R. N., Meenakshi, P. V., Shah, K., Patel, B., Chan, B. P. L., Sunny, S., Chandra, B., Ong, J. J. Y., … Sharma, V. K. (2020). A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak. Brain, Behavior, and Immunity, 88 (April), 559–565. https://doi.org/10.1016/j.bbi.2020.04.049
Cook, G., Burton, L., & Hoogenboom, B. (2006a). Pre-participation screening: the use of fundamental movements as an assessment of function – Part 1. North American Journal of Sports Physical Therapy : NAJSPT, 1(3), 132–139.
Cook, G., Burton, L., & Hoogenboom, B. (2006b). PRE-PARTICIPATION SCREENING: THE USE OF FUNDAMENTAL MOVEMENTS AS AN ASSESSMENT OF FUNCTION – part 2. North American Journal of Sports Physical Therapy : NAJSPT, 1(3), 132–139.
Cools, A. M., Johansson, F. R., Borms, D., & Maenhout, A. (2015). Prevention of shoulder injuries in overhead athletes: A science-based approach.Brazilian Journal of Physical Therapy, 19(5), 331–339. https://doi.org/10.1590/bjpt-rbf.2014.0109
Cornell, S. (2020). FMS Anecdotal Stories.
Jastrzebowski, W. (1857). Ergonomji. Nat. Ind, 2, 29.
Kiesel, K. B., Butler, R. J., & Plisky, P. J. (2014). Prediction of injury by limited and asymmetrical fundamental movement patterns in american football players.
Journal of Sport Rehabilitation, 23(2), 88–94. https://doi.org/10.1123/JSR.2012-0130
Minick, K. I., Kiesel, K. B., Burton, L., Taylor, A., Plisky, P., & Butler, R. J. (2010). INTERRATER RELIABILITY OF THE FUNCTIONAL MOVEMENT SCREEN. https://doi.org/10.1519/JSC.0b013e3181c09c04
Philp, F. (2020). Can we predict injury in male football players based on the functional movement screen and other tests of injury risk? (PhD Academy Award).British Journal of Sports Medicine, <54(9), 558–559. https://doi.org/10.1136/bjsports-2019-100764
Plisky, P. J. (2015). The Relationship Between the FMS and Injury Risk. FMS Website. https://www.functionalmovement.com/articles/649/the_relationship_between_the_fms_and_injury_risk
Rindal, K. (2018). Industrial Athlete Case Study. Vimocity.Com.
Rozmaryn, L. M. (1996). The workplace athlete. Maryland Medical Journal (Baltimore, Md. : 1985), 45(8), 647—654.
Sevier, T. L. (2000). The industrial athlete? [3]. Occupational and Environmental Medicine, 57(4), 285. https://doi.org/10.1136/oem.57.4.285
Tremblay, M. S., Colley, R. C., Saunders, T. J., Healy, G. N., & Owen, N. (2010). Physiological and health implications of a sedentary lifestyle.Applied Physiology, Nutrition and Metabolism,35/i> (6), 725–740. https://doi.org/10.1139/H10-079
Americans with Disabilities Act, 12101 (2008) (testimony of Civil Rights Division U.S. Department of Justice).
Viola, V. A. (2020).EVALUATING THE “INDUSTRIAL ATHLETE” UTILIZING ATHLETIC TRAINERS.


