Analyses of Postures and Musculoskeletal Disorders of Emergency Medical Technicians in the United States
Abstract
The job of emergency medical technicians (EMTs) involves manually handling patients. The force required to safely lift or lower a patient during an emergency response depends on the weight of the patient. These tasks elevate the risk of musculoskeletal disorder (MSD). The objective of this study is to assess the level of MSD risk associated with the most frequently performed tasks of EMTs during emergency response and measure their level of MSD prevalence using a recorded simulation of five frequently performed tasks: (1) stretcher removal, (2) stretcher return with the patient, (3) patient lift: ground to a stretcher, (4) two-person stretcher removal with a patient, and (5) moving a patient down the stairs. Biomechanical and postural assessments are performed using rapid upper limb assessment (RULA) and rapid entire body assessment (REBA). The Nordic Musculoskeletal Questionnaire (NMQ) is used to measure MSD occurrence. Also, a fishbone diagram is developed to determine hidden causes of MSD. Both RULA and REBA scores indicate that Task 3 has the highest MSD risk. The MSD frequency is high in the back (43%) and one or both ankles or feet (21%). Posture, load, and force are three risk factors related to the tasks. Overall, the assessments agree that the most risk is on the lower back. This indicates where ergonomic intervention is needed to reduce the risk of musculoskeletal injury.
KEY WORDS: Biomechanics, EMT, ergonomics, musculoskeletal disorders (MSD), safety
1. Introduction
There are approximately 1,030,760 licensed emergency medical services professionals in the United States, including emergency medical responders and paramedics (National EMS Assessment, 2020). Emergency medical technicians (EMTs) are exposed to various physical and mental risk factors unique to their profession (Rahimi et al., 2015; Jones and Lee, 2005; Lavender et al., 2000). They are exposed to tragic and gruesome events while working in highly-charged emergencies—facing hazards such as assault, violence, and transportation accidents, potentially leading to fatal injuries (Maguire and Smith, 2013; Broniecki et al., 2010; Reichard and Jackson, 2009). Perhaps the most common physical hazards EMTs are exposed to are biomechanical and postural. Working as a first emergency responder has high demands on the musculoskeletal system requiring repetitive motions such as lifting, bending, and twisting (Hong et al., 2010; Aasa et al., 2005; Broniecki et al., 2010; Weaver et al., 2015). Tasks such as moving and transporting patients and performing cardiopulmonary resuscitation (CPR) are some physical stressors to EMTs’ musculoskeletal systems (Studnek and Crawford, 2007).
According to a recent and comprehensive review of work-related MSDs and injuries among EMTs and paramedics (EMTs-Ps), back pain is the most common complaint (Friendenberg et al., 2020). That report found that the annual prevalence of back pain among EMTs-Ps ranges from 30% to 88%. In a study among 180 nurses working as EMTs, about two-thirds had at least one type of back pain (Rahimi et al., 2014). This finding was in congruence with those of the ambulance officers in Hong Kong who reported back discomfort (60%) during CPR (Jones and Lee, 2005). In the United States, data from the Department of Labor’s Bureau of Labor Statistics reported 21,690 cases of non-fatal injuries or illnesses that resulted in lost workdays among EMTs-Ps from 2003 through 2007, and of those, 9,290 (43%) were back injuries (Maguire, 2013). This means that EMTs-Ps have a rate of injury about 3 times the national average for all occupations.
A good number of studies have been conducted to document the prevalence and risk factors of MSDs in EMTs-Ps (Aasa et al., 2005; Jones and Lee, 2005; Lavender et al., 2000; Maguire, 2013; Studnek and Crawford, 2007; Lavander et al., 2007). However, the analyses of biomechanical and postural risk factors that are inherent to this profession have been minimal. To continuously improve the performance and design of ergonomic equipment and processes involved in patient handling during emergency response, there is a need for continuous investigation to understand the tasks performed, including the degree to which these tasks stress the workers and their frequency of performance (Lavender et al., 2000). Also, there must be an analysis of work that describes the postures assumed and the forces applied when EMTs-Ps perform emergency rescue tasks. In ergonomics, task analysis is a common practice used to identify which specific task components expose a worker to ergonomic risk factors and the magnitude of those exposures. In most cases, postural and biomechanical analyses are conducted with the use of a 2D or 3D motion capture system (Schurr et al., 2107).
In this study, the researchers test the effectiveness of typical postural and biomechanical assessment tools that generate levels of MSD risk to provide data that would be used to determine what task component needs the most ergonomic intervention. The researchers hypothesize that the availability of equipment and technology (or the lack thereof) is insufficient to minimize the risk of MSDs and that there are still task components and micro-tasks that may pose cumulative pain and discomfort to the musculoskeletal system of EMTs-Ps. These task components may cause cumulative trauma or acute injuries if not examined thoroughly. The objective of this study is to assess the level of MSD risk associated with frequently-performed work tasks of EMTs during emergency response and measure the level and prevalence of their MSDs.
2. Materials and Methods
2.1 Study Design and Sample
This cross-sectional study is conducted to measure the level of MSD risk faced by emergency medical technicians (EMTs) when performing their tasks during an emergency response. Convenient sampling is used to determine the number of participants with the use of inclusion criteria that includes at least one year of work experience as an EMT at a minimum of 18 years of age. Before data collection and task observation, we excluded those who had previous MSD injuries; we also excluded those who were currently pregnant from the survey. A total of 14 EMTs answered the survey. Three EMTs performed the simulation of patient transfer tasks, and one played the patient. Our research is approved by Keene State College’s Institutional Review Board (IRB) with an assigned protocol number #472.
2.2 Data Gathering Tools
This study uses rapid upper limb assessment (RULA) (McAtamney and Corlett, 1993) and rapid entire body assessment (REBA) (Hignett and McAtamney, 2000) to measure the level of MSD risk associated with each of the frequently performed tasks. RULA evaluates the exposure of individual workers to ergonomic risk factors associated with upper extremity MSD. It considers biomechanical and postural load requirements of job demands on the neck, trunk, and upper extremities. The worksheet generates a single score that represents the level of MSD risk per task and per worker (McAtamney and Corlett, 1993). The score ranges from 1 to 6+, the former having negligible risk and the task requiring no action, the latter having a very high risk with a necessity to implement abrupt change on the task. Also, REBA measures the probability of developing pain or discomfort with the addition of the lower parts of the musculoskeletal system. It accounts for body posture, forceful exertions, type of movement, repetition, and coupling. In the last portion of the evaluation, a score between 1 and 11+ is generated, with 1 having negligible risk and 11+ having very high risk with a need to implement change (Hignett and McAtamney, 2000). Using both MSD assessment tools provides a robust result because it allows cross-validation of findings.
The pain or discomfort of each body region was surveyed through the use of the Nordic Musculoskeletal Questionnaire (NMQ) (Kourinka et al., 1987). The first part of the questionnaire asks for the participant’s job, gender, age, height, weight, length of employment (doing the same job), and hours worked each week. The second section contains a diagram showing the different body regions on a back view, which is used to guide survey participants in answering the NMQ. The questionnaire itself is divided into two columns. Answerable by a “yes” or “no,” Column 1 asks, “Have you at any time during the last 12 months had trouble (ache, pain, discomfort, numbness) in the neck, shoulders (left, right, both), elbows (left, right, both), wrists/hands (left, right, both), upper back, lower back, one or both hips/thighs, one or both knees, and one or both ankles or feet?” Those who answered “yes” in this column have to respond to two more questions, “Have you at any time during the last 12 months been prevented from doing your normal work (at home or away from home) because of the trouble?” and “Have you had trouble at any time during the last 7 days?” An important element of the NMQ is the information regarding how much influence the pain or discomfort had on the worker’s daily routine. The data used in this study is the prevalence in the last seven days.
A root-cause analysis (RCA) is a fundamental, underlying, system-related reason why an incident occurred that identifies one or more correctable system failures (Department of Energy, 1992). It analyzes underlying factors in any given adverse reaction to identify a problem’s source and take corrective measures to fix it. This process is unique as it delves deeper to find answers based on hidden causes and their effects rather than merely looking at the most apparent. Typically, it is considered a reactive process, but when applied thoroughly, it can take the shape of a highly valuable source by becoming a proactive mechanism as it predicts problems before they occur (White, 2022; Bright Hub PM, 2011). In the field of occupational and environmental safety, the Occupational Safety and Health Administration (OSHA) and the Environmental Protection Agency (EPA) urge employers (owners and operators) to conduct an RCA following an incident or near miss at a facility (Department of Energy, 1992).
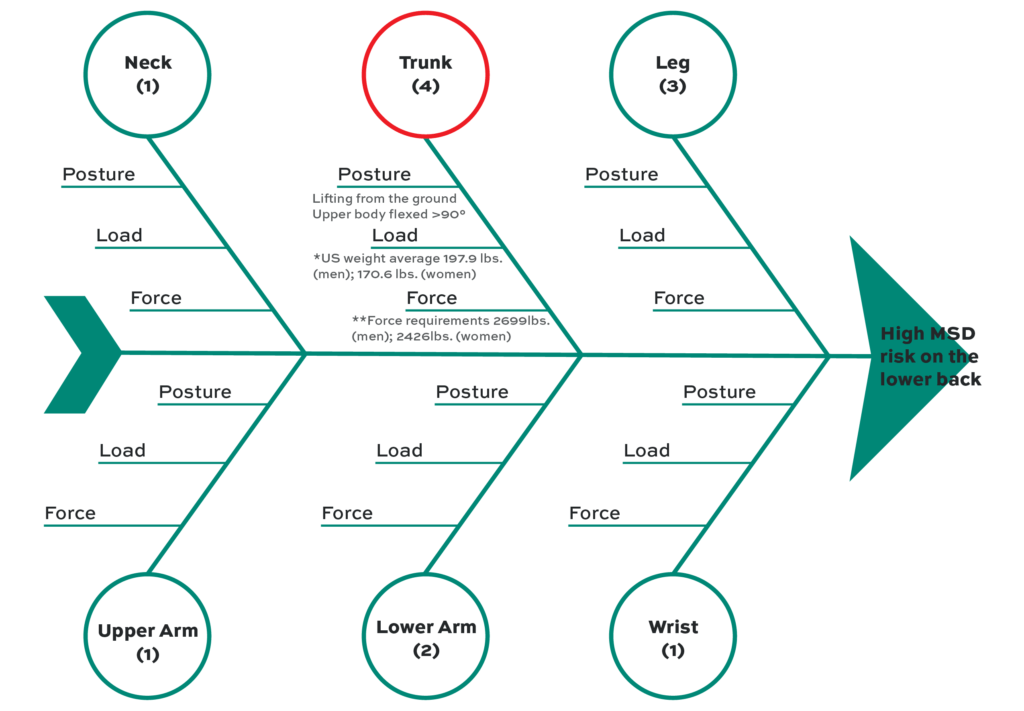
To narrow the cause of hazards for the task that generates the highest RULA and REBA scores, an RCA using a fishbone diagram is performed (Fig. 3). The fishbone diagram is the preferred RCA technique because of its content and visual clarity. It specifies multiple components that have the potential to influence outcomes, which helps prioritize relevant causes. The researchers used the simulated tasks to conduct an RCA. To link the level of MSD risk with RCA, REBA is used because RCA works better with whole-body assessments. The diagram is focused on the body part that has the highest score (trunk). Then, three important factors that influenced the scores are examined: posture, load, and force. For posture, the angle of the upper body while performing the task is assessed. The load is the average body weight in the U.S. based on the findings of Fryar et al. (2018). It is divided between the average weight of men (197.9 lbs.) and women (170.6 lbs.). The force requirement is computed based on a previously described formula for rotational force or moment: M=Weight (W) x Distance (D) (Stack et al., 2016). A moment is defined as the product of the applied force and the perpendicular distance through which the force is applied. The national average of weights and a distance of 10 in, which is the most conservative distance of the load from the lumbosacral joint of the spine during a lifting task, are used in the computations.
2.3 Data Collection Procedures
Following IRB approval, the researchers visited a local EMT company to ask permission to conduct the study. After speaking to the owner and supervisor and receiving approval to survey their workers, the objective of the research, the role of their employees in the study, and the amount of time expected for participation were explained. To protect the privacy of both the company and the employees, the researchers avoided asking for or recording any identifying information. During the first visit to the worksite, the EMTs were gathered to explain the content of the consent form. In considerable detail, they were informed about the purpose of the study, the expectations, potential benefits and incentives, conflicts of interest, confidentiality, their rights as study participants, and their freedom not to participate. The NMQ was handed to those who expressed willingness to support the research and collected the questionnaires within the following week.
In the final visit, the simulation of tasks by three EMTs using a video camera was recorded. One worker acted as a patient, while the other two acted as emergency responders. The tasks were: (1) stretcher removal, (2) stretcher return with patient, (3) patient lift from the ground to the stretcher, (4) two-person stretcher removal with a patient, and (5) moving a patient down the stairs. Figure 1 shows a sample of the five tasks in side and back views. In the first task observed, the workers simulated the removal of a stretcher from the ambulance without a patient on it. This is what they do when they arrive at a scene to recover a patient. For the second task, the first responders showed how they put the stretcher back into the ambulance once the patient is on it. Next, they lifted them from the ground up onto the stretcher (task 3). This represents a situation where the responders show up at the scene with an ambulance that lacks the lifting equipment required for this maneuver. A “two-person stretcher removal with a patient” describes when the EMTs arrive at the hospital with the patient and must remove them from the ambulance (task 4). If the patient is upstairs and the EMTs are incapable of traversing them, they will need to use a piece of equipment (e.g., backboard, stretcher, stairchair, etc.) to transport a patient down the stairs (task 5). These five tasks are a few of the most common work tasks that first responders do when responding to an emergency medical situation (Conrad et al., n.d.). The individual task lasts for 3 to 5 minutes. As it was a simulation, the EMTs explained that the length of time required might vary depending on the anthropometric characteristics, illness, cause of injury of the patient, and sometimes weather conditions. The video clips are used to evaluate the MSD risk using RULA and REBA.

2.4 Data Analyses
The socio-demographic characteristics of the study participants are expressed, in percentage, in terms of sex (male and female). Age, height, weight, body mass index (BMI), year, industry, and hours worked per week are presented in mean and standard deviation. The levels of MSD risk are shown as the original numerical value generated by RULA (1 to 6+) and REBA (1 to 11+). The prevalence of MSD is expressed in percentages. All analyses are performed using Microsoft Excel version 16.59.
3. Results
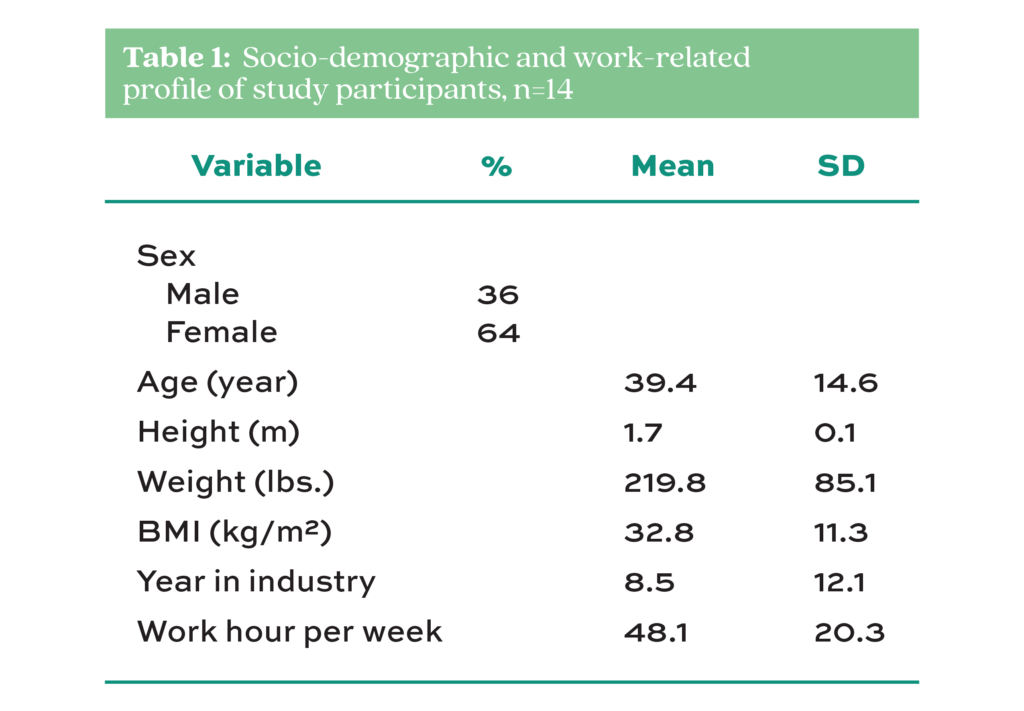
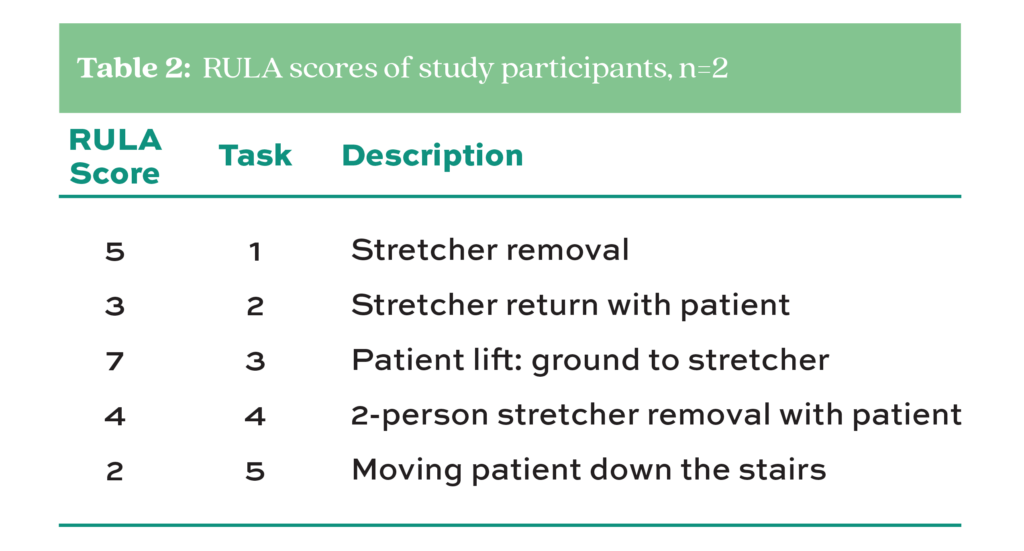
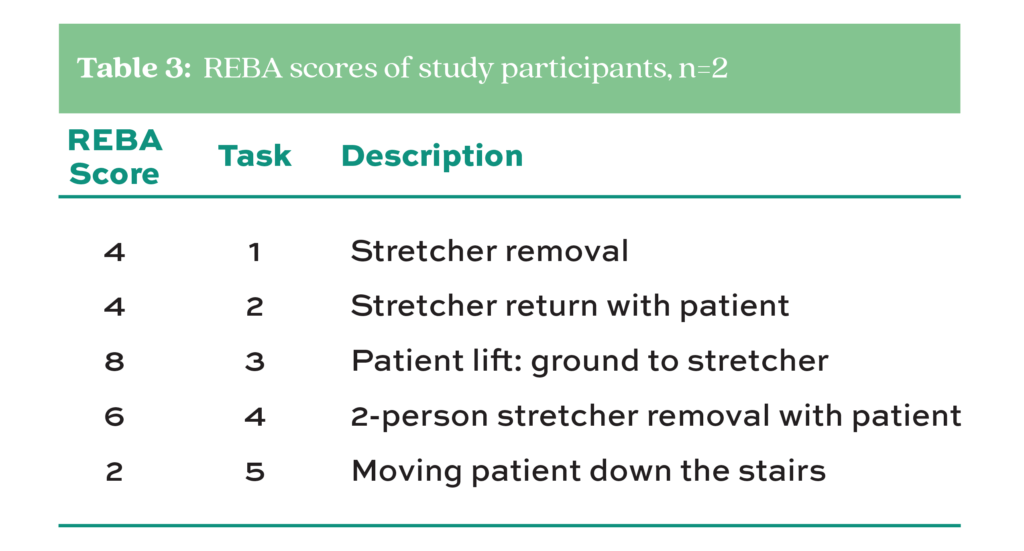
The personal and occupational profiles of the study participants are summarized in Table 1. Among them, 64% are female, and 36% are male. The average age of the EMTs is 40 years, 1.7 m in height, and 219.8 lbs. in weight. The participants’ average BMI is 32.8 kg/m2. In terms of work history, the EMTs work for an average of 9 years with a standard deviation (SD) of 12 years and 48 hours per week with an SD of 20 hours. Table 2 presents the RULA scores of the study participants. It shows that the task with the highest score of 7 is task 3 (patient lift: ground to the stretcher), followed by task 1 (stretcher removal) with a score of 5, and task 4 (two-person stretcher removal) with a score of 4. Task 5 (moving patient down the stairs) has the lowest RULA score of 2. It can be gleaned from Table 3 that the highest REBA score is 8 for task 3 (patient lift: ground to the stretcher), followed by task 4 (two-person stretcher removal with a patient) with a score of 6. The task with the lowest score of 2 was task 5 (moving the patient down the stairs).
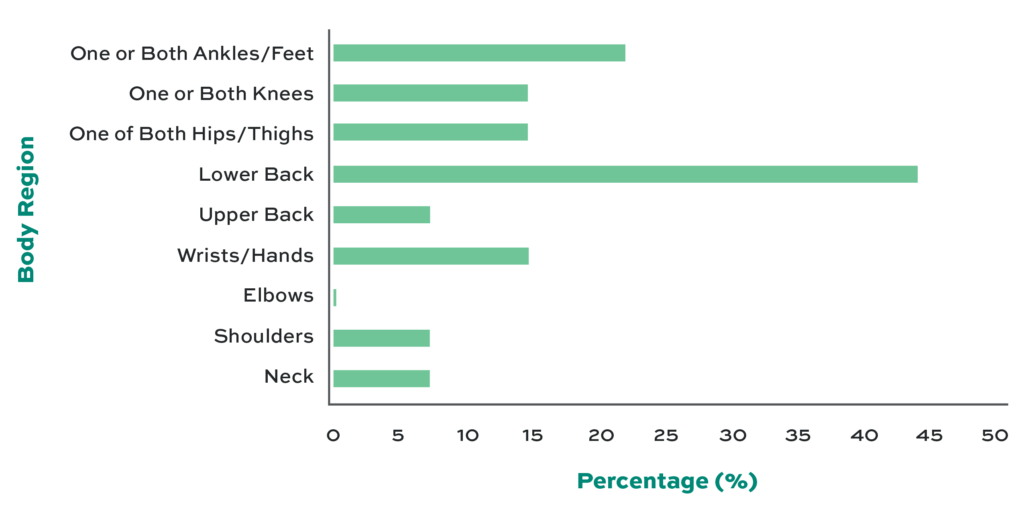
In terms of the prevalence of MSD, Fig. 2 shows that pain in the lower back is the most common (43%). Also, the EMTs reported discomfort in one or both feet (21%), one or both knees (14%), one or both hips (14%), and the wrists (14%). The participants reported no pain in the elbows. The fishbone in Fig. 3 shows the scores received by each body region and the risk factors that influenced them. The risk factors include posture, load, and force requirements that influenced the scores. Among the six body parts (e.g., neck, trunk, leg, upper arm, lower arm, and wrist) evaluated by REBA, the trunk has the highest score of 4, followed by the leg with a score of 3. The neck, upper arm, and wrist have the lowest scores of 1. With posture, the upper body of the EMT is flexed forward to more than 90° while lifting from the ground. The average weight for men in the US is 198 lbs. and 171 lbs. for women. After applying the biomechanical formula (Stack et al., 2016), we found that the muscles generate 2699 lbs. of force for men and 2426 lbs. for women to statically hold patients with the average weights mentioned above.
4. Discussion
This study assesses the postural and biomechanical risks associated with frequently performed tasks of EMTs. It is shown that lifting the patient from the ground onto the stretcher (Fig. 1) results in a high MSD risk, as shown in the RULA and REBA scores (Tables 2 and 3). The result of the NMQ reveals that low back pain is the most common complaint of the study participants in the last 7 days (Fig. 2). This is confirmed by the highest score in the trunk region of the body in the REBA analysis, as shown in Fig. 3. Our findings show that posture, load, and force requirements have negative impacts on the different body regions, but more so on the lower back. This finding should be cause for concern given the relative weights of the patients during an actual response to an emergency and the frequency of exposure of EMTs.
In the present study, there is a 43% prevalence of low back pain among the participants. Low back disorder is the most common form of MSD among health professionals who respond to emergencies (Rahimi et al., 2015; Jones and Lee, 2005; Aasa et al., 2005). Studies show that physical, socio-psychological, and individual risk factors influence this prevalence. Working in awkward postures, lifting a load that is hard to hold, lifting a heavy load (Hansen et al., 2012), CPR procedure, reaching for overhead equipment, and seated tasks that require horizontal bending and twisting (Jones and Lee, 2005) narrow passageways, stairs, and obstacles at the scene, and prolonged flexed and twisted postures (Prairie and Corbeil, 2014) are some of the physical risk factors. Although most of these factors are not investigated in the present study, we believe they contribute to the occurrence of MSD symptoms in the study participants. Other established individual risk factors can include age, physical fitness, being overweight, and a history of back problems. In the present study, the average BMI of the EMTs is 32.8, which is in the obese category, and their average age is 40 years. This means that, on average, the surveyed participants are more likely to develop MSD symptoms. In a study among machine drivers, construction carpenters, and office workers between the ages of 40-45, an increased risk of low back pain (including all types) was found. The symptoms were associated with disc degeneration due to aging (Luoma et al., 2000). Also, prolonged exposure to the above-mentioned physical risk factors has a detrimental effect on the musculoskeletal system, which can be brought about by high call volume, especially when working in an urban setting and depending on the length of career. We found that the study participants worked for 48 hours a week on average. This means that they can be exposed to MSD hazards for at least 8 hours a day.
The RULA and REBA scores show that lifting a patient from the ground to a stretcher (task 3) has the highest MSD risk (Fig. 2). Further analysis reveals that the trunk has the highest score (Fig. 3) among all of the body parts evaluated. Lifting the patient from the ground to the stretcher requires force and proper body mechanics to avoid injuring the back. In the simulation of task 3, the EMT bent his back forward, flexing more than 90°. Apart from that, his source of force came from the back during the peak of the lifting task. The source of force required during lifting directly correlates with the posture followed by the EMT. For instance, if the patient is a 198 lb. man, which is the average weight of males in the US, the erector spinae muscle has to release 2699 lbs. of force to stabilize the lifting task when holding the patient 10 inches away from the trunk (Fig. 3). For patients with an average weight of 171 lbs., the force required to be generated is 2426 lbs. among female EMTs to stabilize the spine during the lifting task. Therefore, the force required is always higher than the weight of the load to stabilize movement during lifting and lowering tasks (Stack et al., 2016). With prolonged exposure, this can be a serious biomechanical risk in the lumbosacral (L5/S1) region of the spine. The farther the load from the lumbosacral region and the more forward flexed the back, the higher the risk of injury.
Removing the need to lift altogether during the patient transfer from the ground to a stretcher is the ideal solution. It’s been proven that transferring and transporting a patient from point A to B with the use of mechanical equipment minimizes the risk of musculoskeletal injuries. Lavender et al. (2007) proved that changing the backboard carrying task to a rolling and sliding task with a mechanical-aided decent control system reduced the demand on the erector spinae muscles, minimized muscle activity in the rectus abdominis, and decreased the rating of perceived exertion. However, ergonomically-designed equipment may not always be available for use and therefore requires EMTs to manually lift and lower patients, as in the case of the study participants in this study.
The findings in this study highlight the need for an ergonomic intervention. We found that knowledge of good body mechanics through ergonomic intervention is necessary to minimize the risk of injury. During manual lifting, awkward posture and overexertion must be avoided. But without proper ergonomic training, the workers may have to sort to what they perceive as normal techniques. Amit and Song (2021) found that significant improvement in workers’ posture can be observed when given ergonomic intervention. The intervention can include awareness of proper lifting techniques, modification of equipment used at work, a healthy lifestyle, and physical activities. The posture of the EMT, the weight of the patient, and the force required in lifting are three of the main factors that influence the REBA scores in the present study. Given that the trunk is exposed to improper posture and high biomechanical loading, it should not be surprising that the NMQ survey indicates the highest prevalence of MSD in the low back region. Given this knowledge, and in the absence of lifting equipment, the EMT should avoid bending forward when lifting. Squatting as a starting posture and maintaining a straight trunk must be observed to utilize the force generated by the legs. This way, lifting or lowering tasks become safer because the capacity of the legs to release force is higher compared to that of the rectus abdominis and extensor muscles. Based on these findings, the need for an ergonomic intervention is warranted among EMTs. Personalizing the intervention by breaking them into specific tasks and movements and considering the personal profiles of the workers (e.g., age, BMI, etc.) can yield better results. The human body can sometimes take time to fully adjust to newly introduced movements. It must be noted, therefore, that getting accustomed to proper lifting techniques and other posture-related interventions must be closely investigated before full implementation.
4.1 Limitations of this Study
There are three major limitations to this study. First, the sample size of the respondents who answered the MSD prevalence survey is small and may not be representative of the emergency medical services profession in the United States. We believe, however, that our findings on MSD prevalence are consistent with those of previously published studies among EMTs and paramedics. To update the existing knowledge on MSDs, we recommend that a survey with a larger sample size be conducted. This can provide important insights into the condition, especially with the fact that most EMT companies are now using state-of-the-art technology and equipment.
The second limitation pertains to the quality of the simulation. Ideally, observations would be obtained from real emergencies. It is anticipated that this can’t be done without interfering with the quality of EMS service. Legal and ethical considerations were also important challenges. We conducted the simulations with the guidance of the EMS manager of the company. The combined expertise of the manager and the workers was used to ensure that the simulated tasks were as close as possible to the generic situations encountered by the personnel. We also anticipate that the improper postures shown by the EMTs may not be representative of the majority of personnel in the industry. The majority may be knowledgeable in proper lifting techniques and may have access to ergonomically-designed equipment. However, we argue that manual lifting can still exist during an emergency response, especially in the absence of such equipment. Therefore, shedding a light on the issue is necessary. Lastly, the design of the study being cross-sectional does not substantially support cause and effect. For future research, we suggest exploring other methodologies that establish a clinical association between the tasks and the condition.
Conflict of Interest
No conflicts of interest to declare.
Acknowledgment
We thank the EMTs and their management for participating in this study, the Center of Creative Inquiry, and the SSH Dean’s Office at Keene State College for the funding.
References
Aasa, U., Barnekow‐Bergkvist, M., Ängquist, K. A., & Brulin, C. (2005). Relationships between work‐related factors and disorders in the neck‐shoulder and low‐back region among female and male ambulance personnel. Journal of Occupational Health, 47(6), 481–489. https://doi.org/10.1539/joh.47.481
Amit, L. M., & Song, Y.-W. (2021). Effectiveness of ergonomic intervention in work-related postures and musculoskeletal disorders of call center workers: A case-control study. Industrial Engineering & Management Systems, 20(2), 109–118. https://doi.org/10.7232/iems.2021.20.2.109
BrightHub Project Management. (2011). A brief history of root cause analysis. https://www.brighthubpm.com/risk-management/123244-how-has-the-root-cause-analysis-evolved-since-inception/
Broniecki, M., Esterman, A., May, E., & Grantham, H. (2010). Musculoskeletal disorder prevalence and risk factors in ambulance officers. Journal of Back and Musculoskeletal Rehabilitation, 23(4), 165–174. https://doi.org/10.3233/bmr-2010-0265
Conrad, K. M. L. (n.d.). Ergonomic study of fire service musculoskeletal injuries. Final performance report. NTIS. https://ntrl.ntis.gov/NTRL/dashboard/searchResults/titleDetail/PB98130776.xhtml
Friedenberg, R., Kalichman, L., Ezra, D., Wacht, O., & Alperovitch-Najenson, D. (2020). Work-related musculoskeletal disorders and injuries among emergency medical technicians and paramedics: A comprehensive narrative review. Archives of Environmental & Occupational Health, 77(1), 9–17. https://doi.org/10.1080/19338244.2020.1832038
Fryar, C. D., Kruszon-Moran, D., Gu, Q., Carroll, M., & Ogden, C. L. (2021). Mean body weight, height, waist circumference, and body mass index among children and adolescents: United States, 1999–2018. https://doi.org/10.15620/cdc:107559
Hansen, C. D., Rasmussen, K., Kyed, M., Nielsen, K. J., & Andersen, J. H. (2012). Physical and psychosocial work environment factors and their association with health outcomes in Danish Ambulance Personnel – a cross-sectional study. BMC Public Health, 12(1). https://doi.org/10.1186/1471-2458-12-534
Hignett, S., & McAtamney, L. (2000). Rapid entire body assessment (reba). Applied Ergonomics, 31(2), 201–205. https://doi.org/10.1016/s0003-6870(99)00039-3
Hong, S. W., Uhm, D. C., & Jun, M. H. (2010). Job stress and work-related musculoskeletal symptoms of 119 emergency medical technicians. Korean Journal of Occupational Health Nursing, 19(2), 223-235. (In Korean)
Jones, A. Y. M., & Lee, R. Y. W. (2005). Cardiopulmonary resuscitation and back injury in ambulance officers. International Archives of Occupational and Environmental Health, 78(4), 332–336. https://doi.org/10.1007/s00420-004-0577-3
Kuorinka, I., Jonsson, B., Kilbom, A., Vinterberg, H., Biering-Sørensen, F., Andersson, G., & Jørgensen, K. (1987). Standardised Nordic questionnaires for the analysis of musculoskeletal symptoms. Applied Ergonomics, 18(3), 233–237. https://doi.org/10.1016/0003-6870(87)90010-x
Lavender, S. A., Conrad, K. M., Reichelt, P. A., Gacki-Smith, J., & Kohok, A. K. (2007). Designing ergonomic interventions for EMS workers, part I: Transporting patients down the stairs. Applied Ergonomics, 38(1), 71–81. https://doi.org/10.1016/j.apergo.2005.12.005
Lavender, S. A., Conrad, K. M., Reichelt, P. A., Johnson, P. W., & T. Meyer, F. (2000). Biomechanical analyses of paramedics simulating frequently performed strenuous work tasks. Applied Ergonomics, 31(2), 167–177. https://doi.org/10.1016/s0003-6870(99)00040-x
Luoma, K., Riihimäki, H., Luukkonen, R., Raininko, R., Viikari-Juntura, E., & Lamminen, A. (2000). Low back pain in relation to lumbar disc degeneration. Spine, 25(4), 487–492. https://doi.org/10.1097/00007632-200002150-00016
Maguire, B. J., & Smith, S. (2013). Injuries and fatalities among emergency medical technicians and paramedics in the United States. Prehospital and Disaster Medicine, 28(4), 376–382. https://doi.org/10.1017/s1049023x13003555
McAtamney, L., & Nigel Corlett, E. (1993). Rula: A survey method for the investigation of work-related upper limb disorders. Applied Ergonomics, 24(2), 91–99. https://doi.org/10.1016/0003-6870(93)90080-s
NASEMSOorg. (2020). NASEMSO releases 2020 National EMS Assessment. ). https://nasemso.org/news-events/news/news-item/nasemso-releases-2020-national-ems-assessment-2/
OSTI.GOV. (1992). Root cause analysis guidance document. DOE guideline. Root cause analysis guidance document. https://www.osti.gov/biblio/10125866-root-cause-analysis-guidance-document-doe-guideline
Prairie, J., & Corbeil, P. (2014). Paramedics on the job: Dynamic Trunk Motion Assessment at the workplace. Applied Ergonomics, 45(4), 895–903. https://doi.org/10.1016/j.apergo.2013.11.006
Rahimi, A., Alhani, F., & Anoosheh, M. (2015). Relationship between low back pain with quality of life, depression, anxiety and stress among emergency medical technicians. Trauma Monthly, 20(2). https://doi.org/10.5812/traumamon.18686
Reichard, A. A., & Jackson, L. L. (2009). Occupational injuries among emergency responders. American Journal of Industrial Medicine. https://doi.org/10.1002/ajim.20772
Schurr, S. A., Marshall, A. N., Resch, J. E., & Saliba, S. A. (2017). Two-dimensional video analysis is comparable to 3D motion capture in lower extremity movement assessment. International Journal of Sports Physical Therapy, 12(2), 163–172.
Stack, T., Ostrom, L. T., & Wilhelmsen, C. A. (2016). Occupational ergonomics: A practical approach. J. Wiley.
Studnek, J. R., & Crawford, J. M. (2007). Factors associated with back problems among emergency medical technicians. American Journal of Industrial Medicine, 50(6), 464–469. https://doi.org/10.1002/ajim.20463
Weaver, M. D., Patterson, P. D., Fabio, A., Moore, C. G., Freiberg, M. S., & Songer, T. J. (2015). An observational study of shift length, crew familiarity, and occupational injury and illness in emergency Medical Services Workers. Occupational and Environmental Medicine, 72(11), 798–804. https://doi.org/10.1136/oemed-2015-102966
White, S. K. (2022). What is root cause analysis? A proactive approach to change management. CIO. https://www.cio.com/article/350219/what-is-root-cause-analysis-a-proactive-approach-to-change-management.html#:~:text=root%20cause%20analysis%3F-,A%20proactive%20approach%20to%20change%20management,to%20reoccur%20in%20the%20future.